How Is Diabetic Retinopathy Diagnosed And Treated
Early diagnosis and treatment of diabetic retinopathy is key to prevent vision loss.
Diabetic retinopathy refers to a condition caused due to the damage to the retina in patients with diabetes. Uncontrolled diabetes can result in the persistently elevated levels of sugar in the blood due to which the light-sensitive part of the eye called the retina is damaged.
If you are suffering from diabetes, read on to learn how diabetic retinopathy is detected and treated.
How is Diabetic Retinopathy Diagnosed?
Diabetic retinopathy, just like diabetes, progresses gradually over a period of time, often without causing any apparent symptoms initially.
Hence, patients with diabetic retinopathy may not experience any symptoms or may have only mild problems with their eyesight.
If not detected and managed early, it can cause blindness. Hence, patients with diabetes are advised to undergo a routine eye check-up so that any damage to the retina can be detected early.

What Will Your Eye Doctor Look Out For During an Eye Examination?
Your doctor will perform a comprehensive dilated eye examination to assess the health of the eyes and your vision.
The exam should be simple and painless. Before the examination, an eye drop will be placed into your eyes to dilate or widen the pupils. This will allow the doctor to view the inside of the eyes more clearly. The drops can cause your near vision to blur for a few minutes. However, the effect would wear off after a few hours restoring your vision.
During the comprehensive eye examination, your ophthalmologist will look for the following signs of diabetic retinopathy:
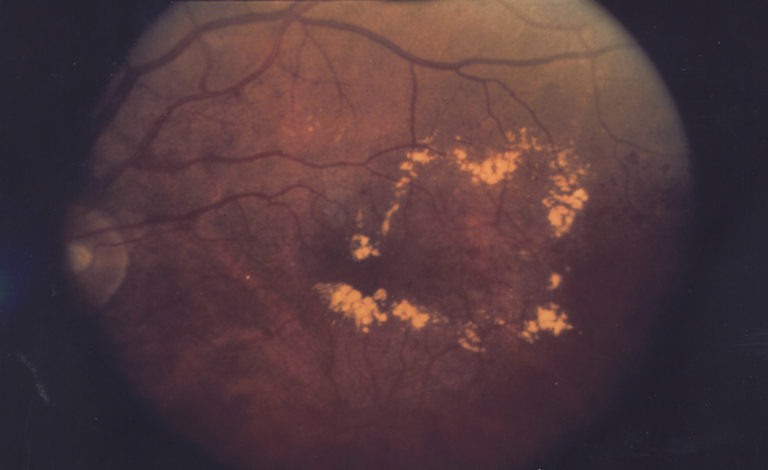
Small red spots in the retina
Small red spots in the retina consisting of small hemorrhages (bleeding) or microaneurysms (bulging capillaries). These are the initial warning signs of diabetic retinopathy that can be detected during a routine eye examination.
Presence of abnormal blood vessels
The detection of abnormal blood vessels in the retinal tissues could be indicative of diabetic retinopathy. Edema (swelling) of the retina with hard exudates (fatty deposits) in the retina is the most common cause of vision loss in diabetes.
Growth of new blood vessels
These signs suggest the body’s efforts to repair the damaged retinal tissues by forming scar and new blood vessels that can supply more nutrients to enhance healing. The new blood vessels can lead to bleeding in the vitreous humor, loss of vision and ultimately even a retinal detachment.
What Are The Other Ways To Examine Diabetic Retinopathy?
As we’ve covered in previous blogs, here are some other methods that can help in the diagnosis and evaluation of diabetic retinopathy.
Fluorescein angiography
This test can be performed during an eye examination with your eyes dilated. It involves capturing images of the inside of the eyes. This is followed by injecting a special dye into the vein of your arm and taking more images once the dye reaches the tissues of the eyes through the bloodstream.
The images, thus captured, can help to identify the blood vessels that are damaged, broken down, closed, and leaking fluid.
This form of examination is an accurate method to determine whether there is adequate blood flow through the blood vessels in the back of your eye. It can also detect vascular changes due to the inner and outer blood-retinal barrier.
Fluorescein angiography can be helpful in observing whether diabetic retinopathy treatment is working. This method of screening can be problematic as it’s an invasive procedure, but at the same time highly effective at detecting any issues in the eye.
Optical coherence tomography
As technology evolves, better cameras and machines become available to help increase early diagnosis in diabetic retinopathy. An optical coherence tomography (OCT) examination is another imaging test that can provide cross-sectional pictures of the retina.
These images provide vital clues about the thickness of the retina to help the doctor assess whether any fluid has leaked into the retinal tissues and caused swelling or edema. OCT examination can also be used to monitor the response of the patient to the treatment of diabetic retinopathy,especially diabetic macular edema.
How is Diabetic Retinopathy Treated?
The treatment of diabetic retinopathy depends on the type and severity of the condition. The treatment is aimed at slowing down or preventing the progress of the condition as explained below.
Early diabetic retinopathy
Patients with mild to moderate nonproliferative diabetic retinopathy may not need active medical intervention. However, your ophthalmologist will likely monitor the health of your eyes and vision on a regular basis to determine when you might need treatment.
In such cases, it is advisable to ensure optimum control over your blood sugar levels and blood pressure so that the progress of diabetic retinopathy can be inhibited.
Advanced diabetic retinopathy
Patients diagnosed with proliferative diabetic retinopathy or diabetic macular edema usually need medical intervention. Depending on the specific changes that have occurred in the retina, the ophthalmologist may recommend one of the following treatments:
Injecting medicines into the eye
The treatment of diabetic retinopathy may involve injecting medications called VEGF (vascular endothelial growth factor) inhibitors into the vitreous of the eye.
These medications help to stop the growth of the new vessels by inhibiting the effects of signals that are sent to stimulate the formation of the new blood vessels. They also reduce vascular leakage and edema formation in diabetic macular edema.
Anti-VEGF therapy is usually a stand-alone treatment but may also be used in combination with other therapies such as photocoagulation.
Photocoagulation
It is a form of laser treatment, also called focal laser treatment, that can prevent or slow down the leakage of fluids in diabetic macular edema.
During this procedure, the part of the abnormal blood vessels through which leakage is occurring is exposed to laser rays.
Focal laser treatment can be performed in the doctor’s clinic, usually in a single session. This treatment may not help to restore the vision completely in patients who have already developed blurring due to macular edema.
Pan-retinal photocoagulation
This is another laser treatment, also called scatter laser treatment, that works by inducing shrinkage of the abnormally formed blood vessels in proliferative diabetic retinopathy.
During this procedure, the part of the retina that is away from the macula is exposed to the scattered laser rays.
This procedure is usually performed in the doctor’s clinic and may require 2 or more sessions. The vision may become blurry for about 24 hours after the procedure. Some patients may develop a loss of night vision or peripheral vision after the sessions.
Vitrectomy
Vitrectomy is a surgical procedure that involves the removal of the Vitreous humor gel that forms nearly 80 percent of the eye cavity and provides a transparent medium through which light can travel inside the eye to reach the retina.
The procedure provides better access to the retina and allows for a variety of repairs, including the removal of scar tissue, laser repair of retinal detachments and treatment of macular holes. During the procedure, a tiny incision is made in the eye. These days, vitrectomy procedures can often be performed with a tiny self-sealing no-stitch inciscion that is about the width of an eyelash.
This procedure is usually performed in a hospital or surgical center under local or general anesthesia.

Regular eye screening
As diabetes is a chronic progressive disorder, retinal damage and the loss of eyesight may continue to worsen in the absence of regular monitoring and treatment.
Patients with diabetes are advised to visit their ophthalmologist on a regular basis to assess their vision and retinal health. Early detection of diabetic retinopathy with the help of advanced diagnostic methods discussed above would help you seek the most appropriate treatment aimed at minimizing the risk of complications like blindness.
Adding risk calculation with the clinically validated RetinaRisk algorithm will further enhance early detection and timely treatment of diabetic retinopathy. RetinaRisk allows for individualized screening for sight threatening diabetic retinopathy.

The RetinaRisk algorithm was developed following extensive international research on risk factors known to affect the progression of diabetic retinopathy, such as the type and duration of diabetes, gender, blood pressure and HbA1c levels, as well as a diagnosis of retinopathy.
Clinical validation in over 25.000 diabetic patients in four continents has confirmed the robustness of the RetinaRisk algorithm. It can predict the risk of retinopathy progression with a very high precision (ROC curve with AUC over 0.8).
Timely diagnosis and treatment of diabetic retinopathy can also help to inhibit the worsening of the condition and enable patients to restore their eyesight, completely or partially, depending on the stage of the disease.
Conclusion
Early detection and proper treatment of diabetic retinopathy, in combination with healthy dietary and lifestyle habits aimed at controlling blood sugar levels, is key to preventing diabetes complications like vision loss or blindness. Make sure that you don’t miss your eye screening this year.