How You Can Lose Your Eyesight to Diabetic Retinopathy if Untreated
Meet Gede. He is 28, lives in Bandung, Java, Indonesia, and has Type 2 diabetes. Gede lost his sight from Diabetic Retinopathy (DR) or diabetic blindness, which could have been avoided. Like other young men and women with diabetes, he did not think he was at risk and didn’t routinely undertake diabetic eye screenings. His sight gradually deteriorated, and when he finally reviewed his diabetic eye reports, it was too advanced to treat.
Admittedly grim. But this is a true story and this bleak outcome can perhaps be attributed to lack of awareness and to some extent, neglect.
If this was not enough, here are some hard facts about the increase of diabetes and population health risks. Obesity, one of the likely causes of diabetes, has risen quickly in the OECD in recent decades and projections indicate that this trend will continue. It is estimated that more than 400 million people in the world have diabetes and this number is expected to exceed 600 million by 2030. In 2016, the World Health Organization (WHO), reported that in Iceland alone, there is a 7.1% prevalence of diabetes and related risks. OECD health statistics for 2017 cite diabetes as one of the top 6 causes for adult mortality. Zoega reported a 0.3% blindness prevalence in diabetic patients in Iceland.
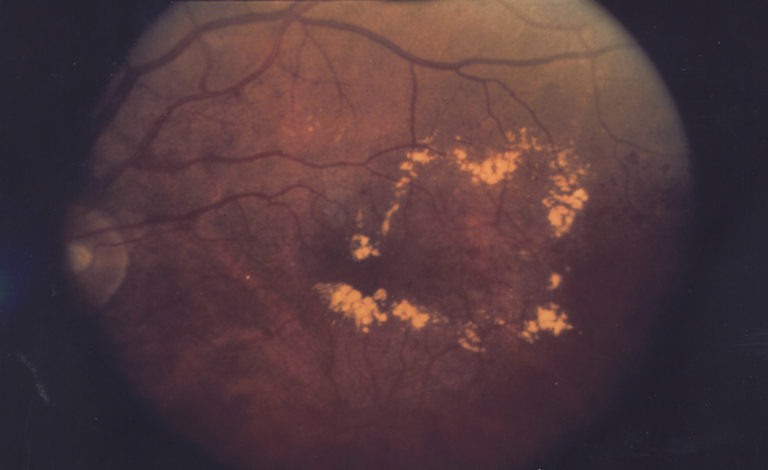
These are alarming numbers and Gede’s story is not the only one. DR, broken down, is a transformation of the retina and if left undiagnosed and untreated, can result in unchangeable visual loss or even blindness. It usually develops several years after the onset of diabetes, and often no symptoms during the early stages of the disease, nor any pain. This often lulls people with Type 1 or Type 2 diabetes to not undergo regular screenings. It’s important, therefore, not to wait for symptoms. When symptoms do occur, they range from mildly blurred central vision to complete vision loss. Symptoms may progress slowly—or rapidly.
Diabetes is the most common cause of blindness amongst working age people in most countries around the world. DR is still one of the most frequent causes of blindness and public health institutions recommend early screenings at frequent intervals for detection and prevention to preserve eyesight. The responsibility of undergoing regular screenings rests with both, the healthcare practitioner and with diabetic individuals. Undertaking regular screenings along with other measures like sugar control minimizes risk, and helps patients receive timely treatment.
Enter Retina Risk.
The Retina Risk App is a unique and novel tool that empowers persons with diabetes to monitor their individualized risk of developing sight-threatening diabetic retinopathy, which is one of the most common causes of blindness world-wide. It is designed by an Iceland-based company founded by academics and health-care providers with over 30 years’ experience in screening for persons with diabetic retinopathy and treating diabetes. It is available, free of charge for mobile device (iOS and Android).
What does this mean?
The risk calculator is based on a mathematical algorithm arrived at after extensive international research on risk factors known to affect the progression of DR, such as duration of diabetes, gender, blood glucose levels and HbA1C. Across several validation studies among different samples of population have confirmed that the algorithm can predict the risk of retinopathy progression with as high as 80% precision.
And in Iceland?
Retina Risk has received significant support from the academic society in Iceland. Founded in 2009 by Professors Einar Stefánsson, MD – Retinal Specialist and Chair of the Landspitali University Hospital Department of Ophthalmology, and Arna Guðmundsdóttir, MD – Diabetologist at Landspitali University Hospital, Department of Endocrinology, it also has a team of specialists in medicine, mathematics, statistics, computer programming, health care economics and business. The University of Iceland and the Icelandic University Hospital contribute significantly.
Managing healthcare records can be a painful experience, for both patients and doctors. Though extensive medical records are kept on patients to be made available to new caregivers, accessing them is not always an easy process and this often results in delays of patient care, or worse, care delivered not based on evidence. There is a better way though. Getting systems to talk to each other is something that Application Programming Interface’s (API) can do very well and can allow patients and healthcare practitioners to access complete healthcare records of a patient to make quicker, easier and more definitive diagnoses and helps patients potentially with an easier and more intuitive interface to access their results.
In Iceland, through the Digi.me, and the Directorate of Health’s API Icelanders can now download their health data on their smart device allowing them to approach healthcare practitioners in a timely manner thereby taking on a much involved and informed role in their healthcare, and we are committed to not having more stories like Gede.